Peripheral Arterial Disease (PAD)
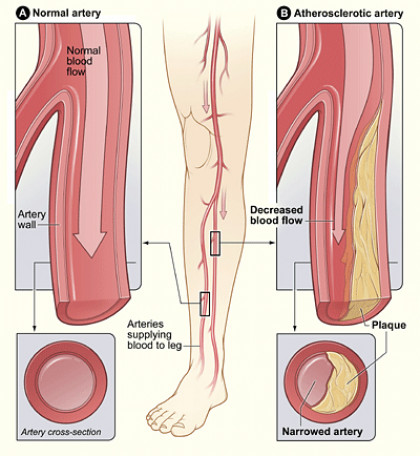
The buildup of cholesterol and plaque in the lining of arteries.
What Causes PAD?
Peripheral arterial disease is caused by atherosclerosis which is the buildup of cholesterol and plaque in the lining of arteries. This process has a genetic basis. It is made worse by factors such as smoking, diabetes and poorly controlled cholesterol and hypertension. In peripheral artery disease (PAD), the plaque buildup causes blood flow restriction to legs and other affected organs. With the progression of PAD induced flow restriction, blood flow cannot keep up with limb’s resting demands for oxygen and nutrients. This causes leg cramps and may lead to non-healing wounds. Arterial blockages are the leading cause of limb amputations due to non-healing leg ulcers/wounds that lead to infection and gangrene. If you have PAD, you are also at higher risk for having heart disease and stroke
Common Symptoms
- Calf, leg or buttock pain (claudication) while walking.
- The pain stops at rest and resumes at a predictable distance.
- Leg weakness, burning or aching feet in feet or toes worse with walking.
- Sores or ulcers on toes, feet or legs that do not heal after four weeks of local wound treatment.
- Change in color or feet, loss of hair and wasting of muscles in the legs.
PAD Treatment
There are several lifestyle changes that can reduce risk of peripheral arterial disease or prevent the disease from getting worse, such as quitting smoking, change in diet, and exercise. The nicotine in cigarettes, cigars or vapes causes damage to the vessel which causes plaque buildup, leading to narrowing or blockages in the arteries. Changes in diet can improve medical conditions such has high cholesterol, diabetes and high blood pressure and reduce risk of peripheral arterial disease. Exercise, such as walking, can improve circulation by creating small collateral vessels around the narrowing or blockage. You should not start an exercise program without consulting your doctor first.
Medical management of arterial disease includes maximally controlling any risk factors that contribute to PAD. This includes treatment of diabetes, high blood pressure, high cholesterol and kidney disease. Cholesterol medication and blood thinners are often prescribed when PAD is diagnosed.
Endovascular treatment involves use of tiny catheters and instruments inserted into arteries through tiny puncture in the groin or leg to treat blocked artery and restore blood flow. This minimally invasive treatment does not require hospitalization or general anesthesia and is performed at an outpatient facility. Techniques used:
Balloon Angioplasty
A catheter with a balloon at the tip is placed across the narrowing and then temporarily inflated, resulting in the opening of the obstructed artery and allowing more blood to flow through.
Stent Placement
A stent is a metallic mesh structure shaped as a cylinder that is delivered to the area of an arterial narrowing or obstruction. This is left in place permanently to restore or increase blood flow. Generally, this is reserved for cases where angioplasty is not sufficient.
Atherectomy
This treatment consists of a specialized catheter that can physically remove fatty and calcified plaques that narrow or obstruct the arteries, restoring blood flow through the diseased artery. Often, this technique is performed in conjunction with angioplasty and/or stenting.
Surgical treatment for arterial disease includes bypass surgery. This is a surgical procedure where a vein or graft is used to create a detour around the block artery.
What is an Angiogram?
Angiography is an X-ray examination that is used to evaluate arteries and veins throughout the body. During the angiogram, Dr. Azher Iqbal inserts a thin tube (a catheter) into one of the arteries through a very small puncture in the skin, about the size of a pencil tip. Contrast (X-ray dye) is then injected into the artery while X-rays are taken of the area. The contrast makes the artery visible on the X-rays.
An angiogram helps interventional radiologists and other doctors plan the best treatment for the patient. One of the most common reasons for an angiogram is to find out if a blocked artery is causing symptoms. For example, a blocked blood vessel in the leg may cause pain when walking; a blocked blood vessel in the kidney may cause high blood pressure.
An angiogram can determine exactly where the blood vessel is obstructed, how severe the blockage is, and what is causing it. Angiography may be needed to supplement other medical tests such as ultrasound, computed tomography (CT) scan, or magnetic resonance (MR).
Frequently Asked Questions
One of the most common reasons for an angiogram is to find out if a blocked artery is causing your symptoms. For example, a blocked artery in the leg may cause pain in your leg when you walk; in the kidney it may cause high blood pressure; and in the brain it may cause vision problems and weakness. An angiogram can determine exactly where the artery is obstructed, how severe the blockage is, and what is causing it. The two most common causes of blocked arteries are a blood clot in the artery and atherosclerosis (hardening of the arteries caused by a build up of plaque).
Another common reason for an angiogram is to see if you have an aneurysm, which is an area of an artery that has ballooned out. Although other medical tests, such as physical examination, ultrasound, computed tomography (CT) scan, or magnetic resonance (MR) can detect an aneurysm, an angiogram may be necessary to see it in detail and to plan treatment.
Angiograms also are used to diagnose difficult problems not resolved by other tests. They are also sometimes used by physicians to help choose the best procedure for you. Before your angiogram begins, a member of the interventional radiology team – the doctor, nurse, or technologist – will talk with you about the procedure in detail and answer any questions you have.
If you are already a patient in the hospital, your nurses and doctors will give you instructions on how to prepare for your angiogram. If you are being admitted to the hospital on the morning of your angiogram, or if you are having your procedure done as an outpatient, follow these instructions, unless your doctor specifies otherwise:
Eating. Do not eat any solid food after midnight on the night before your procedure. You may drink clear fluids.
Medication. Most people can continue to take their prescribed medicines. If you are a diabetic and take insulin, ask your doctor about modifying your insulin dose for the day of your procedure. If you are taking the oral anti-diabetic medicine glucophage (Metformin), you will need to discontinue use for up to 48 hours prior to the procedure and 48 hours following the procedure. Consult with your doctor about blood sugar control during this period. If you take a blood thinner such as Coumadin, you must tell your doctor so that it can be stopped. Bring all your medications with you.
Allergies. If you are allergic to contrast (X-ray dye) or iodine, let your doctor know as soon as possible. If possible, let the interventional radiologist know about your allergy a few days before your angiogram. Your doctors can then plan to take special precautions during the procedure or prescribe special medications prior to the procedure.
Smoking. Do not smoke for at least 24 hours before your angiogram.
Blood tests are usually done the day before the angiogram. Before your procedure, you will dress in a hospital gown and an intravenous (IV) line will be placed in one of your veins. You may need to remove your jewelry, and any dentures or partials. The IV will be used to give you fluids and medicines during the procedure and will stay in place until after your angiogram is completed.
The interventional radiologist will study the X-ray images and discuss the results with your other doctors. Your doctors will work with each other and you to provide you with the best treatment.
If you are already a patient in the hospital, or if you have been scheduled to be admitted to the hospital immediately after your angiogram, you will stay in the hospital after your study is completed. You will return to your hospital room, and the nursing staff will ensure you are all right and that you do not bleed where the catheter was inserted into your artery. They will let you know when you can eat and how long you need to stay in bed.
If you are returning home on the day of your angiogram, you will stay in the hospital for four to six hours after the angiogram is completed. After this observation period, you will be allowed to go home. Have someone drive you home after your procedure. You should not attempt to drive yourself.
After you go home:
- DO resume taking routine medicine except for glucophage.
- DO relax and take it easy for 24 hours.
- DO drink plenty of fluids.
- DO resume your regular diet.
- DO keep a bandage on the catheter insertion site for a day. Put on a dry, clean bandage after bathing.
- DO NOT drive or run machinery for at least 24 hours.
- DO NOT do any strenuous exercise or lifting for at least two days.
- DO NOT take a hot bath or shower for at least 12 hours.
- DO NOT smoke for at least 24 hours.
Call your doctors immediately if:
- You start to bleed where the catheter was inserted. If you begin to bleed, lie down flat and apply pressure on the bleeding area. Your doctor will tell you if you need to return to the hospital.
- There is any change in the color or temperature of the area where the catheter was inserted.
- There is a numbness, coolness or change in color of the arm or leg, where the catheter was inserted.
With modern techniques, angiography is safe and complications are infrequent. However, because the examination includes the use of catheters in your arteries and the use of contrast injection, there is some risk.
Placing a catheter in your artery can damage the artery and may result in bleeding. Even when the artery has not been damaged, you may have a bruise or small lump where the catheter was inserted. The bruise or lump may be sore, but will go away in a few days to a week.
A few patients may get ill from contrast injection. Patients with diabetes, kidney disease or asthma, and those who have had a previous allergic reaction to contrast, tend to get sick more often. If you have kidney disease or are diabetic, asthmatic, or allergic to contrast, let your interventional radiologist know before your procedure begins. Other complications can occur depending on what artery is being studied. The exact risks of your angiogram will be discussed with you in more detail by a member of your interventional radiology team before your procedure begins.
Interventional radiologists are board-certified doctors who specialize in minimally invasive, targeted treatments performed using imaging for guidance. They use their expertise in reading Xrays and using ultrasound, magnetic resonance imaging (MRI), and other diagnostic imaging equipment to guide tiny instruments, such as catheters, through blood vessels or through the skin to treat diseases without surgery.
Interventional radiologists are certified by the American Board of Radiology in both Vascular and Interventional Radiology and Diagnostic Radiology. Your interventional radiologist will work closely with your primary care or other physician to be sure you receive the best possible care.
WHAT OUR
Patients Are Saying
“The staff goes out of their way to assist, answer any questions, and make you feel comfortable. Professional, capable, pleasant.”
Sharon M.
“Treatment has enabled me to want to leave my house and enjoy life again- I can now walk, standup, or sit without constant pain. I was pleased with the polite & professional care. I would recommend Dr. Iqbal to anyone.”
Helen D.
“I recently had the uterine fibroid embolization performed by Dr. Azher Iqbal at Buffalo Vascular Care. It has been made apparent by both Dr. Iqbal and his staff’s actions that the patient is number one. Clearly, this is a highly professional, friendly, efficient team that works cohesively for the total well being of the patient.”
Suzanne P.